Even as a beginner, it is very important for any doctor to have medical interpretation, to make sure their patients understand their questions. With medical interpretation, you will be able to apply the best treatment. It is crucial for patients with limited knowledge of English.
The patients of a medical interpreter often need to have things explained to them in non-technical terms. Therefore, they don’t necessarily need a strict science background.
If you are a beginner in medical interpretation, you will often encounter physiotherapy and occupational therapy appointments. These appointments are excellent for developing your skills in medical interpretation. They require only basic medical interpreter vocabulary and simple instruction sentences. However, it’s still important to prepare for the task by understanding the role of the systems and its components.
As far as the medical interpreter is concerned, it is important that he/she knows the functions of the systems and their components. Self-study is a vital part of interpreting, especially when it comes to medical appointments. As you progress through the systems, you will find that your medical interpretation improves with your understanding of how the body works. This basic knowledge is useful not only in specialist consultations, but also in general consultations.
The following modules correspond to each body system.
All the bodily system
The Respiratory System
The respiratory system contains the lungs on either side and the nose, pharynx, larynx, trachea, and bronchi in the middle. The respiratory system is also known as the respiratory apparatus or ventilatory system. It’s the system responsible for gas exchange in the body. This occurs in millions of tiny air sacs called alveoli. The alveoli have a very rich blood supply, giving the blood close contact with the air. Air is pumped using the respiratory muscles. It enters through the nose or mouth and travels down the trachea. It then flows through the bronchi, and into the secondary and tertiary bronchi.
These are progressively smaller tubes known as the bronchioles. The bronchioles open into the alveoli, allowing for gas exchange. The Respiratory system is responsible for said gas exchange, oration, olfactory (smelling) functions, defense against irritants, clot dissolution, and vocalization.
The Functions of the Respiratory System
The respiratory system has several basic functions. These include:
- Gas exchange: The lungs take in oxygen and expel CO2 and other waste gasses.
- Local defenses: When nerve endings in the nose and throat are irritated, the lungs contract in a cough reflex. This expels the irritant or trapping it in the mucous along the inside of the trachea. The mucus is then coughed out or swallowed.
- Clot dissolution: Fibrinolysis is the process that prevents blood clots from growing and becoming problematic. The lungs contain a fibrinolytic system to dissolve clots (or embolisms) that have arrived in the pulmonary circulation.
- Vocalization: Air movement through the larynx, pharynx, and mouth allows humans to speak. Our vocal folds (located in the larynx) require this movement to vibrate and produce sound.
Common Respiratory Diseases and Maladies
The respiratory tract is particularly prone to illness as it’s in constant contact with irritants in the outside world. Here are a few of the most common respiratory system diseases and maladies you may encounter during interpreting assignments:
- Asthma: The most common chronic respiratory condition, asthma causes difficulty breathing due to airway inflammation. Symptoms include dry cough, wheezing, and shortness of breath. Asthma often presents in childhood.
- Chronic Obstructive Pulmonary Disease (COPD): COPD is an umbrella term that covers several disorders, diseases, and maladies. These maladies cause breathlessness or the inability to exhale normally. COPD is most generally caused by smoking or exposure to smoking.
- Bronchitis: An example of COPD is chronic bronchitis, characterized by a chronic cough with sputum (mucus from the lungs). This cough presents especially in the morning.
- Emphysema: Another example of COPD is emphysema. In this case, smoke or other irritants have damaged the air sacs in the lungs. The irritants damage the air sacs to the point where they can no longer repair themselves.
- Lung Cancer: lung cancer can be difficult to detect as it can develop in any part of the lungs. DNA mutations in the cells cause them to multiply and form abnormally. This creates tumors that interfere with respiratory function. Lung cancer is the leading cause of cancer death among both men and women in the US.
- Cystic Fibrosis/Bronchiectasis: Cystic fibrosis is a genetic respiratory disease. A defective gene creates thick, sticky mucus that clogs up tubes and passageways. This causes repeat, severe lung infections. Cystic fibrosis also affects the pancreas, causing obstructions that prevent enzymes from breaking down nutrients. People with cystic fibrosis also develop bronchiectasis. Bronchiectasis is a condition in which the bronchial tubes are abnormally dilated. Mucus pools in the extra space and causes infections, wheezing, and shortness of breath. Bronchiectasis is possible to contract without cystic fibrosis and it’s more prevalent in women than men.
- Pneumonia: Pneumonia is a common illness caused by infections (bacterial, fungal, or viral) in the air sacs in the lungs. Symptoms include cough, fever, shaking, chills, and shortness of breath. Children and seniors are most prone to pneumonia due to their lowered immune status.
- Pleural Effusion: Pleural effusion occurs when fluid collects between the lung and the chest wall. The fluid can collect for a number of reasons, including congestive heart failure, cancer, or pneumonia. Symptoms include chest discomfort and shortness of breath.
The Muscular System
The muscular system consists of skeletal, smooth, and cardiac muscles. It permits movement, strength, blood circulation, posture maintenance, and temperature regulation/heat production. Muscles can be either controlled through the nervous system or completely autonomous, such as cardiac muscle.
What are muscles?
There are three types of muscle present in the human body:
- Skeletal Muscle: Skeletal muscle is a form of striated muscle tissue, meaning that it grows in lines. More accurately, it grows in long, tubular cells called muscle fibers, composed of sarcomeres and myofibrils. These are arranged into bunches known as fascicles. Skeletal muscles are voluntary muscles. They’re controlled by the nervous system and move as a response to “action potential:” neural stimulation. The muscle fibers are attached to bones by bundles of collagen, known as tendons. There are roughly 639 skeletal muscles in the body.
- Cardiac muscle: Cardiac muscle is another form of striated muscle. It differs from skeletal muscle in that the muscle fibers are attached to each other, rather than to bone. Cardiac muscle is an involuntary muscle, meaning that it works automatically. Cardiac muscle cells, also known as cardiomyocytes, contract to pump the heart. Cardiac muscle cells contain many mitochondria, more than skeletal muscle. The mitochondria produce adenosine triphosphate (ATP) at high quantities so that the muscles are resistant to fatigue.
- Smooth muscle: Smooth muscle is an involuntary, non-striated muscle. Smooth muscle cells are found in the walls of hollow organs, including the intestines, stomach, bladder, and uterus. They’re also found in passageways–such as veins, arteries, and the tracts of the respiratory, urinary, and reproductive systems.
Muscular System Specialists
Specialists who work with muscles are called Rheumatologists. Rheumatologists work not only with muscles but with tendons, joints, bones, and nerves that are experiencing inflammation. As we mentioned in the introduction, you’ll likely also work with physical and occupational therapists. They work not only with muscles, but with bones, joints, tendons, and nerves. Their goal is to improve quality of life, range of motion, strength, and recovery. There are a number of common muscular injuries you may encounter:
- Muscle strains: muscle strains are contraction-related injuries in which muscle fibers tear due to extensive stress. They most often occur during acceleration or deceleration, like sprinting or jumping. They range from mild to severe. A mild strain indicates that only a few fibers have been torn. A severe strain is categorized by a complete tear or rupture into two distinct parts. They can occur either from the tendon or in the middle of the muscle.
- Muscle contusions: Contusions, or bruises, are usually the direct result of a hard blow to the muscle. This causes muscle damage and bleeding, forming a hematoma visible beneath the skin as discoloration.
- Muscle cramps: Cramps are caused by involuntary over-shortening or contractions. They’re categorized by mild to excruciating pain and often an inability to move the affected limb. They typically occur in the thighs, calves, hamstrings, or feet. Though they’re painful, they are not considered dangerous to long-term muscle use. They typically clear on their own within minutes, but sometimes take several days for pain to completely subside.
- Muscle Soreness: Muscle soreness is most common during exercise. If it occurs after exercise, it’s referred to as Delayed Onset Muscle Soreness, or DOMS. DOMS is classified as a grade 1 muscle strain injury. It is most commonly seen in individuals who exercise sporadically, or without proper warm-ups. The soreness is thought to be a result of inflammation that occurs during the muscle repair process.
The Skeletal System
The skeletal system is the internal framework of the human body, comprised of around 300 bones at birth. This number decreases to about 206 bones by adulthood as some fuse together as we grow. Babies have more bones than adults as their skeletons haven’t fully developed. This means that they’re naturally more flexible and able to curl inside the womb. The extra cartilage instead of bone also makes it easier for mother and child during the birthing process.
Cartilage turns to bone during a process called “Ossification.” Capillaries (tiny blood vessels) deliver oxygen-rich blood to osteoblasts, the cells that form bones. The osteoblasts create bone to cover the cartilage and eventually replace it, leaving fused bones.
The skeleton serves six major functions through our entire lives: Support, Movement, Protection, Blood cell Production, Storage, and Endocrine Regulation. Human skeletons are divided into two bone categories: the axial skeleton and the appendicular skeleton.
Skeleton Crew: Bone Specialists
In medical interpretation, you’ll most typically encounter the three most common bone specialists: Orthopedists, Osteopaths, and Chiropractors.
- Orthopedics is a surgical specialty and orthopedists work with bones, joints, tendons, muscles, and ligaments. They provide both surgical and non-surgical repairs and treatments for pain and injuries. Orthopedic surgeons hold an MD (medical doctorate).
- Osteopathy is a system of healthcare that takes a more “whole body” approach to healing. It’s a non-surgical approach that focuses on stretching and massage to increase mobility and relieve tension. Osteopaths study primary care medicine and often work as family physicians. Osteopaths can specialize in any area and frequently categorize themselves as internal medicine practitioners. Osteopaths hold a DO (doctor of osteopathy degree).
- Chiropractors focus on the relationship between the nerves, muscles, and skeleton. Chiropractic treatment tends to be more spine and joint focused than osteopathy. It’s often comprised of small spinal adjustments to better align bones and relieve joint pain and pressure. Chiropractors hold a DC (Doctor of Chiropractic degree).
Common Skeletal Maladies and Injuries
As an interpreter, you’ll be more commonly working with patients experiencing an injury or other dysfunction. Here are some of the most common skeletal maladies and injuries you might encounter while on the job:
- Fractures: Fractures include a wide variety of subsets covered under two broad categories: simple and compound. A simple fracture is when the bone cracks but doesn’t split in two. A compound fracture is when the bone splits entirely into separate pieces. Fractures are treated with splints, casts, or less commonly, traction. If severe enough, surgical intervention might be necessary.
- Dislocation: This is the most common injury for athletes. Dislocation occurs when the bone’s joint couldn’t handle the force upon it, causing the bones to move out of position.
- Osteoarthritis: Arthritis is a broad term used to describe joint pain and dysfunction. Osteoarthritis results from the breakdown of joint cartilage and underlying bone.
- Bone Spur: Also known as Exotosis, a bone spur occurs when new bone forms on the surface of an existing bone. This can cause pain ranging from mild to severe. They typically form on the joints and grow upwards.
- Multiple Myeloma: MM, or Plasma Cell Myeloma, is a type of cancer that frequently presents as bone pain and lesions. It’s considered treatable with chemotherapy, steroids, targeted therapy, and stem cell transplants. Bone lesions may be treated with radiation therapy.
- Osteoporosis: Osteoporosis is a condition where bone loss and weakening lead to a greater risk of bone fractures. Osteoporosis is the most common reason for broken bones among the elderly. The most common osteoporotic fracture easily visible in the elderly is a vertebral collapse. This is also known as a compression fracture. It causes a curved back and posture as well as chronic pain with a reduction in mobility.
- Osteomyelitis: Osteomyelitis is a bone infection, usually bacterial but sometimes fungal. It presents as bone pain, redness, fever, and weakness. It’s most commonly found in the long bones of the arms and legs in children. In adults, it presents or in the spine, hips, and feet.
- Fibrous Dysplasia: in cases of Fibrous Dysplasia, normal bone and marrow are replaced with fibrous tissue. This new bone is weak and prone to expansion, causing deformity and pain. Treatment is mostly palliative, focused on pain and fracture management.
The Circulatory System
The circulatory system’s functions can be divided into two categories: cardiovascular and lymphatic. The cardiovascular system’s main objective is to circulate blood in a closed system. This transports nutrients, oxygen, carbon dioxide, hormones, and blood cells throughout the body. The system includes the heart, arteries, veins, and capillaries with “guest appearances” by the lungs, kidneys, and digestive tract. The lymphatic system is made of lymphatic vessels: organs, and tissues whose purpose is to carry lymph towards the heart. Lymph is the fluid between all cells in the body’s tissues. The lymphatic system is responsible for the return of fluid between blood vessels and cells to central circulation.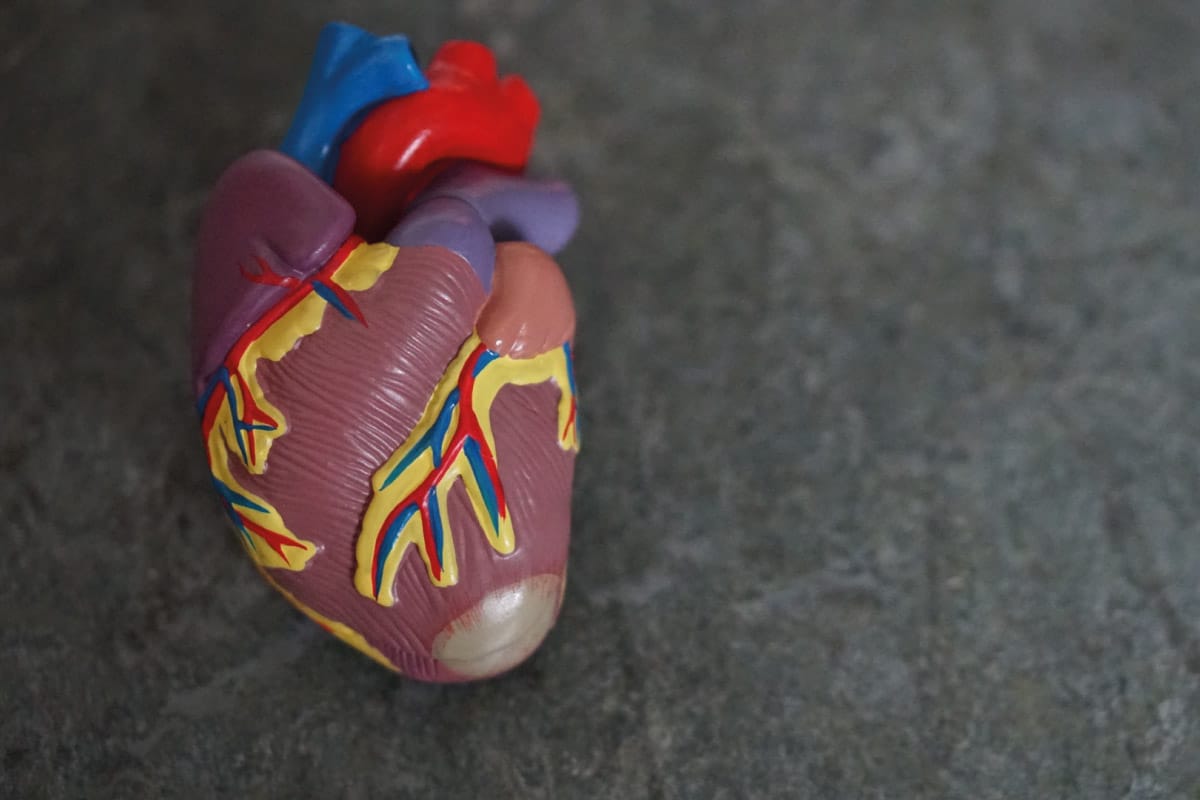
The Path of Blood through the Circulatory System
When the heart contracts, blood follows a specific pattern through the pulmonary and then systemic circuits. It goes through the following steps:
- Deoxygenated blood starts its journey through the pulmonary circuit. Deoxygenated blood is blood that’s exchanged its oxygen for carbon dioxide during its trip through the circulatory system. The blood enters either the superior or inferior vena cava and arrives in the right atrium.
- The deoxygenated blood drains through the right atrium and into the right ventricle. From here, it’s pumped into the pulmonary artery.
- The pulmonary artery takes the deoxygenated blood through the lungs, where it becomes oxygenated.
- The newly oxygenated blood returns to the heart through the pulmonary veins and enters the left atrium. This starts its path through the systemic circuit.
- The blood drains to the left ventricle, where it’s then pumped through the aorta.
- The aorta branches out into smaller arteries, which branch out into smaller arterioles, which branch out to capillaries. The blood starts to engage in capillary exchange. This is the process by which cells exchange carbon dioxide and other waste for oxygen and nutrients.
- The capillaries carry the carbon dioxide and waste through the deoxygenated blood, to small veins called venules. Venules branch out and expand into veins, which carry the deoxygenated blood to the largest veins–the vena cavas. The process begins again.
Common blood diseases and disorders
Hematology is the study of blood in health, disease, and diagnostics. A medical doctor with specialized knowledge about blood is called a hematologist. The most common blood disorders and diseases are categorized into three groups:
- Anemias: Anemia is the most common blood disorder. It includes several types, including nutritional anemias (directly caused by nutritional deficits or disorders. Anemias also include non-nutritional varieties (anemias not directly caused by nutritional deficits or disorders). Anemia is a decrease in red blood cells or less than the normal quantity of hemoglobin in the blood. This means that oxygen can’t be properly transported through the bloodstream.
- Blood Cancers: Blood cancer is defined as any cancer that affects or involves the blood, bone marrow, or lymph nodes. It’s also referred to as hematological malignancy. This includes leukemias, lymphomas, and myelomas.
- Coagulopathy: Any condition in which the blood’s ability to coagulate, or form clots, is impaired. This impairs the body’s ability to heal itself and can cause prolonged and/or internal bleeding. A well-known example is Hemophilia, a genetic coagulopathy disorder.
The Gastrointestinal System
The gastrointestinal system is also known as the excretory system, digestive tract, alimentary canal, and GI tract. It is the organ system that takes in food, processes the nutrients, and expels waste.
The GI tract includes all organs between the mouth and anus to form a continuous passageway. The purpose of this passageway is to take in and digest food, then expel waste in the form of feces. The entire human GI tract is roughly 30 feet long at autopsy. However, in the living body, the intestinal muscles are in a constantly half-tense (contracted) state. The Gastrointestinal system also contains trillions of microbes. These present in the form of over 4,000 strains of bacteria that aid in digestion, metabolism, and immune health.
How does food move through the digestive tract?
Food moves through the digestive system in a process known as peristalsis. Peristalsis describes the series of wave-like muscle contractions that start in the esophagus and continue through the anus. Peristalsis isn’t reliant on gravity. This is how astronauts can eat in space. The path of food through the digestive follows this pattern:
- Mouth: Digestion begins in the mouth. Salivary glands produce saliva to start breaking down simple sugars. Chewing happens to make food easier to process. When you chew food, you instinctively form it into a ball, or “bolus” in the mouth. This makes it easier to swallow. The tongue pushes the bolus into the throat. The epiglottis, a fold of tissue at the back of the throat, closes over your windpipe to prevent choking. The food passes into your esophagus.
- Esophagus: The esophagus is where the digestive process becomes automatic. The brain signals the muscles in the esophagus and peristalsis begins.
- Lower Esophageal Sphincter: Once the food reaches the end of the esophagus, the esophageal sphincter relaxes. This allows the food to move into the stomach.
- Stomach: The stomach muscles mix the food with acidic digestive juices to further break it down. After it’s thoroughly mixed, the stomach contents (called chyme) empty into the small intestine.
- Small intestine: Muscles in the small intestine further mix food with digestive juices from the liver, pancreas, and intestine itself. The walls of the small intestine are covered in villi. These are small, finger-like protrusions that absorb water and facilitate the transfer of digested nutrients into the bloodstream. Peristalsis continues and food moves into the large intestine.
- Large Intestine: The large intestine (or colon) processes waste from the digestive process: undigested parts of food, older cells from the digestive tract, and excess fluid. The large intestine absorbs water and helps compact the remaining waste into solid stool. Peristalsis moves the stool into the rectum.
- Rectum: The rectum is the lower end of the large intestine. It stores the stool until it’s pushed out through your anus in the form of a bowel movement.
- Anus: The stool is pushed through your anus in the form of a bowel movement.
Gastro specialists and maladies
A doctor who specializes in disorders, maladies, and injuries to the gastrointestinal system is known as a gastroenterologist. There are a number of common gastrointestinal maladies you might encounter as an interpreter:
- Gastroesophageal Reflux Disease (GERD): Also known as acid reflux, GERD presents as a burning pain in the chest, typically after meals or at night.
- Gallstones: Gallstones are hard, pebble-like bits of material that form in the gallbladder. They’re typically composed of cholesterol or bilirubin (the compound that gives feces its brown hue). They range in size from a grain of sand to a golf ball. They’re resolved with medications or, in extreme cases, surgical intervention.
- Celiac Disease: Celiac disease is a genetic, serious sensitivity to gluten (a protein found in wheat, rye, and barley). When someone with Celiac eats gluten, it triggers an immune response that attacks the villi in the small intestine. Symptoms vary from person to person. They may include bloating, nausea, vomiting, pain, diarrhea, constipation, depression, bone loss, anemia, fatigue, and weight loss.
- Crohn’s Disease: Crohn’s disease is one of a group of digestive conditions known as IBD (irritable bowel disease). Crohn’s affects the terminal ileum: the part of the colon that connects the small intestine to the large intestine. Current estimates put the number of Americans experiencing Crohn’s Disease at over 810,000 in 2021. Symptoms include abdominal pain, bloating, rectal bleeding, weight loss, and fever. Treatment includes topical pain relievers, immunosuppressants, and sometimes surgery.
- Ulcerative Colitis: Classed with Crohn’s disease as an IBD, Ulcerative Colitis affects solely the large intestine. Symptoms include frequent and urgent bowel movements, bloody stool, pain with diarrhea, and abdominal cramps.
- Irritable Bowel Syndrome: Also known as IBS, Irritable Bowel Syndrome causes constipation or diarrhea, unpredictable stool consistency, bloating, and pain. An estimated 10-15 percent of people worldwide live with IBS. Treatment largely centers around dietary changes and varies from person to person depending on their needs and sensitivities.
- Hemorrhoids: Hemorrhoids are an inflammation of the blood vessels at the end of the digestive tract. They’re often painful and itchy and can cause bright red blood in stool. They’re often accompanied by anal fissures, as the two share causes: constipation, straining, and diarrhea. While Hemorrhoids present with inflammation, anal fissures are tiny, oval-shaped tears in the intestinal lining of the anus. The most common treatment for both is to add more fiber to your diet.
- Diverticulitis: Diverticula are small pouches that form anywhere there are weak spots in the digestive tract–most often in the colon. If the pouches become inflamed, they’re known as diverticulitis. Symptoms include abdominal pain and fever. Mild diverticulitis is treated with fluids and antibiotics so your intestine can heal. Severe diverticulitis can require surgery to remove the damaged part of the intestine.
The Integumentary System
The Integumentary system, also known as the skin system, is one of the most common terminology groups you’ll encounter. Dermatologist appointments are common, whether for less-severe maladies or cancer screenings. The integumentary system comprises the skin and related appendages, like hair and nails. It has a variety of functions. These include protecting the body from damage, and excreting wastes, regulating body temperature.
The skin also provides for vitamin D synthesis and acts as an attachment site for sensory receptors. These receptors detect pain, sensation, pressure, and temperature.
The Structure of Skin
Skin is the largest organ of the human body, accounting for 12-15% of total body weight. It’s composed of two major layers: the superficial epidermis and deeper dermis. These, in turn, are made up of smaller layers to form the full structure.
- Epidermis: The epidermis is the layer of skin that you see when you look at someone. It’s composed of 4-5 layers of epithelial cells and is avascular. This means that there are no blood vessels that reach into it. Epithelial cells in the top layers (all the layers before the bottom layer of the Epidermis) are keratinocytes. Keratinocytes manufacture and store keratin. Keratin is the fibrous protein that gives skin, hair, and nails its hardness and water resistance. The skin cells in the epidermis are constantly being sloughed off and replaced by deeper cells. These cells are, in turn, regenerated in the deeper layers and pushed up.
- Papillary Region: The Papillary region is the first layer of the dermis. It’s composed of loose connective tissue and is named for its fingerlike projections (the papillae). The papillae interlock with the bumps in the lowest layer of the epidermis to form a stronger connection. In the fingers, palms, soles, and toes, the papillae also project the ridges adopted by the epidermis. The epidermal ridges form in patterns that are visible on the surface of the skin–fingerprints.
- Reticular Region: The reticular region is located below the papillary region and is the thickest layer. It’s composed of dense, irregular connective tissue. It holds the roots of hairs, sebaceous (oil) glands, sweat glands, receptors, nail bases, and blood vessels. Tattoo ink and stretch marks are also held in the reticular region.
- Hypodermis: This is also known as the subcutaneous tissue. Thee hypodermis isn’t technically a part of the skin but attaches the skin to underlying bone and muscle. It also supplies the skin with blood vessels and nerves. The Hypodermis is composed of connective tissue, elastin, and adipose tissue (fat). The fat serves as padding and insulation for the body.
Common Maladies and Diseases of the Integumentary System
Dermatologists are the doctors responsible for handling maladies, diseases, and injuries that affect the skin. They handle everything from acne to skin cancer and are vital health professionals. As dermatology appointments are quite common, you’ll likely encounter some of these maladies in your career as an interpreter.
- Acne: Acne occurs when the passageways that connect the skin’s pores to the oil glands become clogged. Acne can occur anywhere on the body and is frequently seen on the face, neck, shoulders, chest, back, and buttocks. The most common forms are whiteheads and blackheads. More severe forms of acne include nodular and cystic acne. Treatment includes topical creams, steroid injections, and occasional minor surgery to remove cysts.
- Cold Sores: Cold sores are red, fluid-filled blisters that generally form around the mouth. They’re caused by a virus known as herpes simplex and are highly contagious through skin to skin contact. While there’s no cure for cold sores, they can be treated fairly easy with over-the-counter creams and antiviral ointments.
- Contact Dermatitis: Contact Dermatitis appears hours to days after contact with an allergen. It’s distinct from other forms of dermatitis. There are clear edges to the rash which correspond to where the allergen came in contact with the skin. Contact Dermatitis usually clears on its own. It can be helped with hydrocortisone cream and antihistamine pills.
- Eczema: Eczema is characterized by red, itchy rashes and dry skin. It’s categorized into three types. Atopic dermatitis is genetic, most common, and typically forms in the crux of the elbows and behind the knees. Allergic contact dermatitis occurs when the rash appears after contact with environmental factors such as jewelry, cosmetics, and fragrances. Nummular dermatitis presents as red and flaky coin-shaped patches, due to dry skin. Eczema is most often treated with corticosteroids and moisturizing creams.
- Psoriasis: Psoriasis is a skin condition that causes buildup of excess skin tissue with a red, thick, scaly appearance. It usually first appears on the elbows and knees but can spread to other areas of the body.
- Rosacea: Rosacea is characterized by facial redness, small bumps, skin sensitivity, skin flushing, and skin dryness. It’s subtyped into four groups. Subtype one (ETR) is associated with facial flushing, redness, and visible blood vessels. Subtype two (papulopustular) is associated by acne-like breakouts. Subtype three (rhinophyma) is rare and involves a thickening of skin on the nose. Subtype four (ocular) is rosacea centered around the eye area. There are no known cures for rosacea. However, a doctor can help create a treatment plan based around eliminating flare-ups.
- Seborrheic Dermatitis: Also known as cradle cap, seborrheic dermatitis mostly affects babies up to six months old. It presents as an oily, crusty, flaky patch on the scalp. It usually clears on its own as the child grows and is occasionally seen again during puberty.
- Skin cancer: Skin cancer is the most common cancer in the United States. Basal and Squamous cell carcinoma are the most common. However, 75% of skin-cancer-related deaths occur due to melanoma. Skin cancer is most commonly treated by excising the affected area and occasionally combining the excision with chemotherapy.
The Nervous System
The nervous system is where everything “comes together,” so to speak. It reaches from our major organs to the tips of our fingers. Neural impulses control everything we do and work with the rest of our body to facilitate movement, sensation, and balance.
The nervous system coordinates actions and sensory information by transmitting signals to and from different parts of the body. This happens via an extraordinarily complex neural map. The nervous system then works in tandem with other systems of the body to respond to the stimulus. The cells that make up the nervous system are called neurons. Neurons send electrochemical impulses through the body, rapidly and precisely, and back to the brain’s own neural network.
Types of Nerves in the Human Body
There are over seven trillion nerves in the human body that can be classed into four categories: cranial, motor, sensory, and autonomic.
- Cranial nerves: These are twelve pairs of cranial nerves originate at the underside of the brain. They include the olfactory, optic, oculomotor, trochlear, trigeminal, abducens, facial, vestibulocochlear, glossopharyngeal, vagus, spinal accessory and hypo glossal nerves. These are essential in vision, smell, eye and facial movements, salivation, and tongue movements.
- Motor Nerves: Motor nerves send impulses from the brain and spinal cord throughout the body to stimulate movement. Motor neurons allow people to do it all: from blinking to walking to talking to dancing and everything in between.
- Sensory Nerves: Sensory nerves transmit information in exactly the opposite direction from motor neurons. Instead of sending impulses from the brain to the body, sensory neurons collect information from the body. They send it back to the spinal cord and the brain.
- Autonomic Nerves: Autonomic (you can think of them as “automatic”) nerves regulate the activity of automatic muscle processes. These include heartbeats, peristalsis, and glands. The autonomic nervous system includes two subcategories. The sympathetic nervous system regulates heartbeat, fight-or-flight response, and other similar impulses. The parasympathetic nervous system regulates digestion, excretion, and other metabolic activities.
Common Nervous System Disorders and Maladies
A neurologist is the medical professional responsible for diagnosing nervous system disorders and diseases. Here are some of the most common maladies you might encounter on assignment as an interpreter:
- Dementia: Dementia is a general term for a group of degenerative conditions, most commonly seen in the elderly. The most common of these is Alzheimer’s disease, which attacks the brain cells and neurotransmitters. This affects how the brain’s able to process and store information. Alzheimer’s presents with speech difficulty, forgetfulness, difficulty with performing everyday routines, and mood and personality changes.
- Bell’s Palsy: Bell’s Palsy is the weakness or paralysis of one side of the face. It’s caused by damage to the facial nerve or general inflammation and usually clears without treatment within 3-9 months. Bell’s palsy can also cause a drooping eyelid/difficulty closing one eye, headache, sensitivity, difficulty eating, drooling, and loss of taste.
- Cerebral Palsy: In cerebral palsy, nervous system damage (localized in the motor cortex) before, during, or after birth impairs muscle control. The condition affects coordination, muscle tone, movement, and posture. It’s also associated with impaired speech, vision, hearing, learning, and eating. It is not degenerative but there’s no known cure.
- Epilepsy: Epilepsy is a broad term for a range of nervous system disorders that cause repeated seizures. These seizures may be triggered by stress, sounds, light, smells, or another stimulus. It’s a treatable disorder, with medication and trigger avoidance.
- Motor Neuron Disease: Motor Neuron Disease, also known as MND, amyotrophic lateral sclerosis (ALS), or Lou Gehrig’s disease, affects the neurons. This causes muscle weakness that leads to paralysis. MND has no known cure, but doctors focus on maintaining mobility and muscle control for as long as possible.
- Multiple Sclerosis: Also known as MS, Multiple Sclerosis is a chronic disease that affects the myelin sheath. MS causes scars or lesions in the nervous system and impairs neural communication. MS typically starts with mild symptoms that build as the damage extends. The most common symptoms include a lack of muscle control, loss of coordination and balance, sensitivity to heat. MS can also present with tiredness, vertigo, dizziness, incontinence, personality and mood changes, and inability to concentrate. There is no known cure, but medicines are often prescribed to ease the symptoms and delay progression.
- Sciatica: Sciatica is a condition characterized by pain in the back, buttocks, and legs. It’s caused by injury, bone spurs or growths, spinal canal narrowing, or tight and swollen muscles in the buttock. Symptoms include pain, numbness, and tingling in the leg. Mild sciatica typically goes away on its own with rest. More severe forms may require physical therapy, lifestyle changes, and anti-inflammatory medications.
- Parkinson’s Disease: Parkinson’s disease is caused by damage to the nerve cells in a region of the brain that produces dopamine. Dopamine is a chemical vital to smooth muscle movements. Parkinson’s mainly affects people who are 65 or older but early onset is possible. Parkinson’s presents as muscle weakness, shaking (often in the hands), muscle rigidity or stiffness, stooped posture, and balance problems. It can also cause depression, memory loss, forgetfulness, and insomnia. There is no known cure. Treatment options include medication to substitute or increase dopamine, lifestyle changes, and (in some cases) brain surgery.
The Immune System
The immune system is certainly integral but also arguably different from other systems. While the skeletal or circulatory system include easily identifiable components, the immune system is so much more. The immune system is everywhere. It combines all of the systems in an incredible dance to keep us healthy and safe.
The immune system is the vast, complex, beautiful, and frankly magical collection of structures and processes that protect us from disease. It works with every other system of the body to keep us healthy. To function properly, the immune system must be able to distinguish between pathogens and healthy tissue. “Pathogen” is a broad term for anything that can cause disease, such as viruses and parasitic worms. As pathogens have the ability to rapidly evolve, the immune system’s defense mechanisms must also constantly learn and evolve. The study of the immune system and its components is called Immunology.
How The Immune System Fights Disease
The immune system fights disease in a process known as the “immune response.” For this example, let’s cover one of the most common forms of immune response processes: fighting a bacterial infection.
- Injury: You’re walking outside and you trip and fall, cutting yourself on something sharp. Ow! Your body’s first form of protection, your skin, has been breached. Nearby bacteria enter the wound.
- Bacteria Grow: The bacteria use the body’s resources to grow and reproduce. At first, the body doesn’t notice them. However, as their numbers continue to swell, the bacteria start to change the environment around them, causing damage.
- Macrophages Intervene: The macrophages (guard cells) intervene. Each macrophage can ingest up to 100 intruder cells each. Once ingested, the intruder cells are trapped in a membrane, broken down by enzymes, and killed. This is often enough to suffocate an attack. The macrophages also send messenger proteins throughout the body to cause inflammation. This is extra water release into the area to make fighting easier. If the macrophages are unable to handle the infection themselves, they release messenger proteins. The messenger proteins communicate the urgency and location of the infection.
- Neutrophils Arrive: Neutrophils arrive and generate barriers that trap and kill bacteria. To kill the bacteria, they release toxins that also cause peripheral damage to healthy cells. Neutrophils are so toxic that they’re designed to die after five days. This reduces the damage they do to healthy cells while also killing bacteria.
- Dendritic Cells Activate: If the macrophages and neutrophils aren’t enough, the macrophages send chemical messages to the dendritic cells. The dendritic cells activate and start collecting signals from the invaders. They rip the signals apart and present them on the cell membrane like trophies from battle. The dendritic cells make a vital decision: Should they call for anti-virus forces or bacteria killers? In this case, the antibacterial army is necessary.
- T-Cells Enlist: The dendritic cells travel to the nearest lymph node (it usually takes about a day) and enlist the help of t-cells. T-cells (a specially trained lymphocyte) have distinct configurations. The dendritic cells look for T-cells with the configuration they need to fight the infection. They determine this by seeing which T-cells react properly with the invader signals the dendritic cell membranes present.
- T-Cells Duplicate: When the dendrite locates the right T-cell, the T-cell duplicates thousands of times. Some become memory cells for if this infection returns. Some travel to the site of the infection to help out. Finally, some travel to the center of the lymph node to activate the B-cells.
- B-Cells Duplicate: When B-cells meet T-cells with the same configuration, the B-cells start rapidly duplicating and producing antibodies to fight the infection. The T-cells stimulate the B-cells for as long as the infection is still present. Then they stop, allowing the B-cells to die from exhaustion so no bodily resources or energy is wasted.
- Antibodies Arrive: The antibodies produced by the B-cells travel to the infection site and bind to the surface of the intruder cells. They stun the remaining bacteria and render them helpless or dead. Helpless bacteria are an easy target for the macrophages. The macrophages can more easily consume the intruder cells after the antibodies have attached.
- Infection is Wiped Out! The infection is wiped out! The healthy body cells that have died as collateral damage are quickly replenished. Most of the immune cells involved in the battle now die to avoid using unnecessary bodily resources. However, the memory cells stay behind. if this type of bacteria is encountered again, the body will be able to handle it quickly and effectively.
Immune System Diseases and Disorders
You’ll encounter a number of common immune diseases during medical interpretations. As we mentioned in the overview, the study of the immune system is immunology. You’ll generally work with patients through the diagnosis process. This starts with a general practitioner visit and then escalates to an immunologist if necessary. Here are some of the most common immune system disorders and diseases:
- Severe Combined Immunodeficiency (SCID): SCID is a condition present at birth that causes the immune system to either be inactive or have limited function. Children with SCID are missing crucial white blood cells. They have to be quarantined to protect them from diseases and infections.
- Temporary Acquired Immunodeficiencies: Temporary acquired immunodeficiencies happen when the immune system is weakened by a variety of possible factors. These include certain medicines, flu, mononucleosis, organ transplants, smoking, alcohol, and poor nutrition. The immune system typically recovers with rest and medical supervision.
- AIDS: HIV, the cause of AIDS, is a viral infection that destroys white blood cells and weakens the immune system. People with HIV/AIDS become extremely ill from sicknesses that healthy immune systems can fight off. These infections are called “opportunistic infections.”
- Asthma: Asthma is the result of an overactive immune system triggered by pollutants and allergens in the lungs.
- Atopic dermatitis: Atopic dermatitis, a form of eczema, is the result of an overactive immune system. The system attempts to attack allergens and instead damages healthy cells and causes inflammation.
- Type 1 Diabetes: Type 1 Diabetes is an autoimmune disorder in which the immune system attacks the cells in the pancreas that make insulin. Insulin is the hormone that removes sugar from the blood to use as energy.
- Rheumatoid arthritis: Rheumatoid arthritis is a common autoimmune disorder that causes joint swelling and deformity. It happens when the immune system attacks the cells in and around the joints.
- Lupus: Lupus is another autoimmune disease in which the immune system attacks healthy cells in various parts of the body. This happens most commonly in the lungs, kidney, and skin.
Most Common Scans
In medical interpretation, two of the most common appointments you’ll attend will be scan-prep and scans themselves. Providers can order a scan at any time during a general or specialist appointment—or occasionally, even over the phone.
What are the Most Common Scans You’ll Encounter as an Interpreter?
When a provider orders scans, it should never be a full surprise to the patient. The provider should explain their reasons for ordering the scan as well as the scan procedure in detail. While this explanation should be in clear language, it’s always useful as an interpreter to have background information and knowledge. Here are some simple explanations for the most common scans you’ll encounter as an interpreter.
Common Scans types:
- X-Ray:
- An X-Ray (often called a radiograph) uses electromagnetic radiation that passes through soft tissue and is absorbed by hard tissue (like bones). The X-Ray film develops much like camera film: showing the areas exposed to radiation and where the radiation was absorbed in stark contrast.
- CT Scan:
- Also known as a CAT scan (Computerized Axial Tomography), CT scans evolved from Tomographs. Tomographs are multiple x-rays taken at different levels to check the depth of an abnormality. The CT scan uses multiple x-ray beams projected at many angles in conjunction with computer resources. The result is a three-dimensional cross-sectional image. Each image reveals a different level of tissue that resembles “slices.”
- MRI:
- Magnetic Resonance Imaging is also known as nuclear magnetic resonance imaging. MRIs differ from CT scans and X-rays in that there’s no exposure to radiation during the scan. MRIs use two powerful magnets (one external and one internal) that align the hydrogen proton “spins” in the body. The scanner also produces a radio frequency current that creates a varying magnetic field. The protons absorb the energy from the magnetic field and flip their spins. When the field is turned off, the protons gradually return to their normal spin, a process called precession. The return process produces a radio signal that is measured by receivers in the scanner and made into an image. The machine captures the image and processes it with a computer. Contrast is often intravenously pumped during the scan and provides more dynamic images.
- PET scans:
- Positron Emission Tomography is a scan that measures the metabolic activity that occurs in body tissue. The scan works by detecting concentrations of photons emitted by radionuclides. For example, in PET scans of the brain, a radioactive atom is applied to glucose (blood sugar). This is because the brain uses glucose for its metabolism. This process creates a radionuclide called fluorodeoxyglucose (FDG). FDG is widely used in PET scanning. Before being scanned, a patient abstains from eating carbohydrates for 12-24 hours. Directly before the scan, they drink a glucose concoction with these radioactive atoms. Contrast is often intravenously pumped during the scan. Because cancer cells metabolize more glucose than healthy cells, the image shows the higher concentrations of glucose metabolism. The higher concentrations on the image indicate where cancer is most likely found.
- Ultrasounds:
- Ultrasound machines transmit high frequency sound pulses into the body with a probe. The sound waves hit boundaries between tissues (for example, fluid and soft tissue, soft tissue and bone). The sound waves are reflected at different depths/boundaries and are picked up by the probe and relayed to the machine. The machine calculates the distances between the different boundaries. Then, it displays the distances and intensities on a screen, showing a two-dimensional image.
Most Common Specialist Appointments
Most medical interpreters start their careers with simple appointments: physical therapy, occupational therapy, individual/talk therapy, and well/sick visits. By the time you’re interpreting for specialist appointments, you should be fairly well-versed in general interpreting procedure. You’ll have a system down for learning vocabulary and you’ll know what to expect from a general medical visit. Though it may seem daunting to take this next step, specialist appointments are very much in the same vein.
Take some time before the appointment to review vocabulary you’ll likely use. This vocabulary is often body system-specific: we’ll talk about the bodily systems in future blogs in this series. In some ways, a specialist appointment is easier to prepare for than a general interpreting assignment. You have a general idea of what the provider and patient need to discuss as it’s localized to one system.
Always ask your project manager or site contact for any information they’re able to give before the assignment. With specialist appointments, this is especially necessary: there might be vocabulary particular to the non-English speaker’s condition. Remember: all vocabulary you learn, even specialized vocabulary, is an investment! Once you’ve learned it, you’ll be able to use it for future assignments. Studying for specialist appointments also gives you the advantage of further understanding how bodily systems work together in detailed ways.
Preparing for an Assignment with a Medical Specialist
At Global Arena, our interpreters provide service for a wide variety of appointments and needs. While the majority of our assignments fall into the “common medical appointments” category, experienced interpreters regularly receive specialist work. Here are the most common specialist appointments to which we assign medical interpreters:
- Cardiologists: Cardiologists work with disorders of the heart and circulatory system.
- Dermatologists: Dermatologists handle maladies and injuries of the integumentary (skin) system.
- Endocrinologists: Endocrinology is the branch of medicine that studies and handles hormones and hormonal disorders.
- Gastroenterologists: Gastroenterologists work with patients who are experiencing disorders, illnesses, and injuries that affect the digestive (or excretive) system.
- Geriatricians: Geriatric doctors work with the elderly population. Geriatrics is also a subset of Family and Internal Medicin
- Gynecologists: Gynecologists work with the female reproductive system, including well visits/check ups, diagnostics, pregnancy visits and scans (obstetrics), fertility and menstruation, STIs, hormone disorders, and treatment of reproductive disorders and diseases.
- Nephrologists: Nephrologists help patients who are experiencing kidney disease.
- Neurologists: Neurologists work with disorders of the nervous system, including both central and peripheral nervous systems and all of their components.
- Oncologists: Medical oncologists diagnose and treat different forms of cancer. They often work closely with other specialists for a whole-body approach to monitoring and treatment.
- Orthopedists: Orthopedists and orthopedic surgeons handle bone disorders, diseases, injuries, and maladies.
- Psychiatrists and Psychologists: There’s a big difference between psychiatrists and psychologists. Psychiatrists prescribe and handle medication and psychologists use psychotherapy to help ease and treat emotional and mental pain. Psychiatrists and psychologists work together to treat mental disorders.
- Pulmonologists: Pulmonologists handle respiratory diseases and disorders as well as lung abnormalities.
- Urologists: Urologists work with the urinary tract and often work closely with nephrologists.
Medical Terminology for Interpreters: an eLearning course by Global Arena
Want to learn more about medical terminology, anatomy, and physiology? Are you pressed for time, and need to be able to take a course at your own pace? Global Arena’s eLearning course, Medical Terminology for Interpreters, gives foundational medical knowledge for all interpreting skill levels. It provides a basic overview of common providers, appointments, scans, procedures, and the bodily systems.
The course is timed for three hours and includes a mix of interactive, informative, and review slides. Upon successful completion of all reviews, you’ll receive a Certificate of Course Completion worth three CEUs. The course meets CCHI and NBCMI standards for interpreter training and counts towards your credit hours for exam pre-requisites. You’ll also receive our Medical Terminology glossary, complete with spaces to add vocabulary in your target language. The course is updated regularly, and registration includes lifetime access to all new information and materials. Learn more and sign up today!






